CareFirst Administrators
Frequently Asked Questions
Does our plan offer gym membership discounts or other wellness discounts?
If you are enrolled in the Trust medical plan, you are Blue Cross and Blue Shield (BCBS) member. As a BCBS member, this gives you exclusive access to healthy deals and discounts through Blue365. With Blue365, great deals are yours for every aspect of your life – like discounts on brand name sneakers, heart rate monitors, and gym memberships! Register now at www.blue365deals.com to take advantage of Blue365. Just have your Blue Cross and Blue Shield member ID card handy. In a couple of minutes, you will be registered and ready to shop.
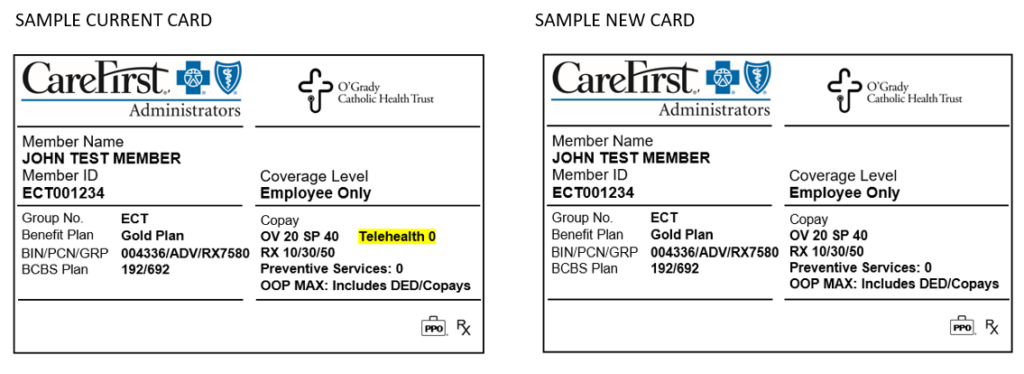
Will I receive a new medical ID card after open enrollment (for the 2021 plan year)?
Yes. CareFirst Administrators will send you a new ID card for your 2021 medical plan, even if you do not change medical plans. This will come in a plain white envelope. Be sure your mailing address is up to date with your employer to prevent delays in obtaining your new card.
The reason for this decision, is due to confusion that could arise due to the current card showing “Telehealth 0.” The new card removes this piece of information because of the varying telehealth benefit as outlined below.
For MDLIVE Providers:
MDLIVE telehealth visits have the $0 copay for Platinum, Gold, & Silver plans, or Deductible then $0 copay for the Bronze plan.
- During the national health emergency (through 12/31/2020) the deductible is waived for the Bronze plan for MDLIVE visits.
For Non-MDLIVE Providers:
The standard office visit benefit applies for virtual or telephonic visits with providers for clinical staff of primary care, general practice, internal medicine, pediatrics, OBGYN and associated nurse practitioners only, during the national health emergency, through 12/31/2020. Starting 1/1/2021 the plan will cover virtual and telephonic visits with all non-MDLIVE providers at the applicable office visit benefit (including specialists).
How is testing and treatment of COVID-19 covered by my medical plan?
At the outset of the pandemic, the Trust elected to waive member cost share for treatment related to COVID. As average daily COVID-19 cases and hospitalizations continue to drop amid widespread vaccine adoption, we’re at an important turning point for our country and community. CareFirst Administrators has revisited with the Trust some of the benefits we enacted at the height of the pandemic.
Effective September 1, 2021, the Trust is ending member cost share waivers for COVID-19 treatment. Providers may collect the appropriate member cost share (copay, coinsurance, and deductible) for treatment rendered on and after September 1, 2021.
In keeping with local and federal requirements, the cost share waiver (that means no cost to members) will continue for the duration of the public health emergency (through May 11, 2023):
- Visits (in all settings) associated with diagnostic COVID-19 testing
- Diagnostic COVID-19 tests
- FDA-authorized COVID-19 antibody tests
Beginning May 12, 2023 member cost share for these services will be applied.
The COVID-19 vaccination is not considered preventive treatment and will remain at zero cost share for members.
I was billed by my provider for expenses I do not think I should have been billed for. Who should I contact for help with this?
Health Advocate’s experts will take on virtually any healthcare or administrative issue so you get to the right care at the right time at no cost to you. If you’ve received a bill or have a claim that you need help with, call Health Advocate at 866.799.2728 or email answers@healthadvocate.com to have your own personal health advocate tackle the issue for you! If authorizations are required to resolve your inquiry, the Advocate assigned to your case will send you any required authorizations forms electronically.
How do I read my medical EOB (Explanation of Benefits)?
Since an EOB isn’t a bill, what you pay is for your information only. If you owe the doctor, or hospital, they’ll send you an invoice. Comparing the EOB and the invoice is a good way to make sure you’re getting billed correctly by the doctor or hospital.
Not all claims generate an EOB. For example, you won’t get an EOB for a prescription. EOBs show you the costs associated with the services you received, including:
- Claim Details, each service or procedure from each provider is explained
- What the provider charged
- What the allowed charges are (this is the contracted amount in which an in-network PPO provider agrees to accept as payment)
- Any non-allowed charges (discount or amount billed over the contracted amount for this service)
- What the Plan pays
- Total covered
- What you pay (summary of Deductibles, copays, and coinsurance)
How do I change my address for my benefits through the Trust?
Contact human resources or your benefits manager to have your address updated for all of the Trust plans you are enrolled in.
How do I find a doctor, hospital, or urgent care center near me?
It’s easy to find the doctors you need at www.cfablue.com.
Select the Members tab on the top right-hand side of the screen.
Select Search Providers under Find a Doctor on the left-hand side of the screen.
Select Find a Doctor under Medical.
Enter your Location then enter ECT as the plan prefix.
Click on the Continue button.
Select one of the search options: Doctors by name, Doctors by specialty, Places by name, or Places by Type.
Populate the search field(s) with your search criteria. Click the magnifying glass icon, or hit the enter key to review a directory based on your search criteria.
How do I request a new medical ID card?
Log in to the CFA member portal at www.cfablue.com. Click the Request ID Cards tile. Follow the instructions and click Submit my Request. You’ll receive a replacement member ID card in 7-10 business days. Need one sooner? On the CFABlue home page, click on the Digital ID Card tile. Follow the instructions to view and print your ID card.
If you are unable to log into the CFA member portal, please contact CFA member services at 877.889.2478. Once your identity is verified, a member services representative will be able to order a new card for you.